Adhesive capsulitis, better known as frozen shoulder, is a condition of unknown cause. It affects 2-5% of the population, with certain risk factors, such as a previous shoulder injury or diabetes, increasing the likelihood of developing the condition.
Fortunately, adhesive capsulitis will usually resolve itself. The timescale for this however, can be long, ranging from 9 months to 3 years. The vast majority of people will achieve a full functional recovery, but some may still experience mild stiffness and occasional pain.
The shoulder joint is, by design, incredibly mobile.
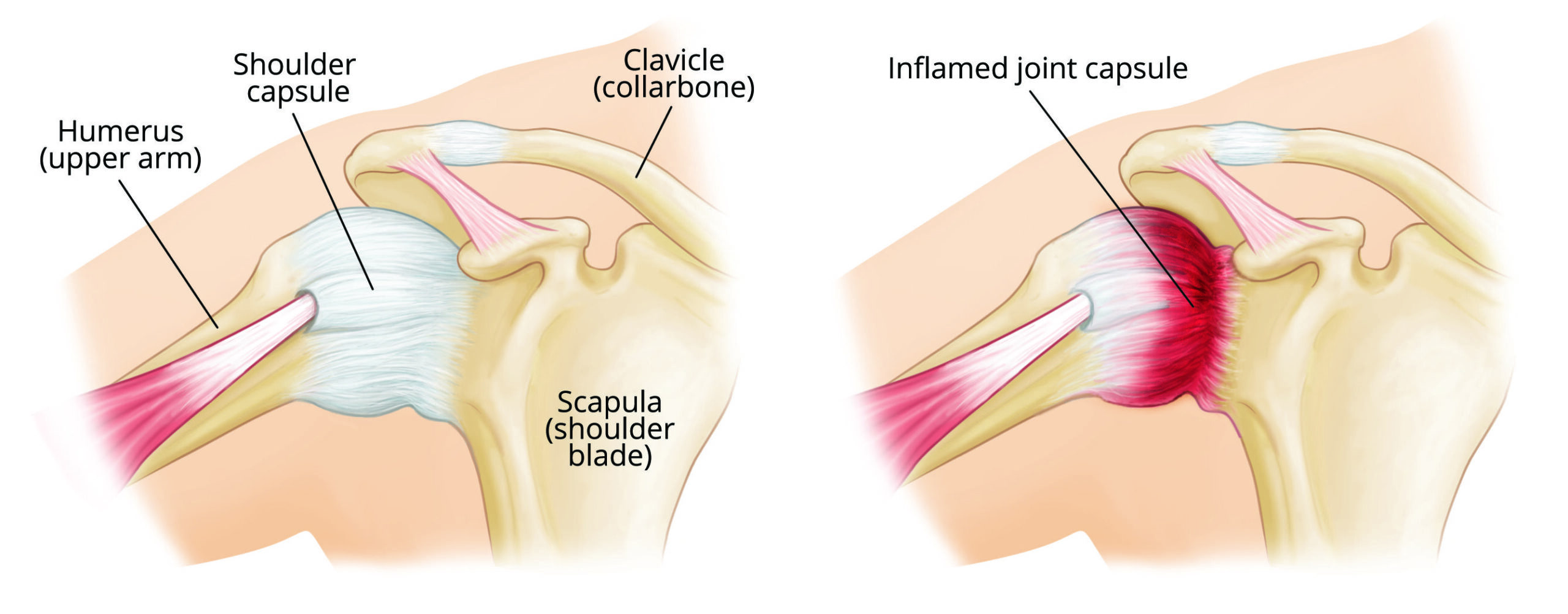
Surrounding the joint, as with other joints of the body, is a capsule. The role of the capsule is to provide stability, sensory information, and aid in lubrication of the joint.
The capsule of the shoulder is very large and baggy, allowing you great flexibility. Tightening of this joint capsule is what causes a frozen shoulder.
SYMPTOMS
The typical symptoms of adhesive capsulitis”
- Pain and stiffness.
- Night time pain can be one of the first indicators of developing a frozen shoulder.
- Stiffness will then begin with difficulties lifting the arm to your side, behind your back and rotating it outwards.
In frozen shoulder, the shoulder capsule thickens and becomes stiff and tight. Thick bands of tissue — called adhesions — develop. In many cases, there is less synovial fluid in the joint.
The hallmark signs of this condition are severe pain and being unable to move your shoulder — either on your own or with the help of someone else. It develops in three stages:
Stage 1: Freezing
In the “freezing” stage, you slowly have more and more pain. As the pain worsens, your shoulder loses range of motion. Freezing typically lasts from 6 weeks to 9 months.
Stage 2: Frozen
Painful symptoms may actually improve during this stage, but the stiffness remains. During the 4 to 6 months of the “frozen” stage, daily activities may be very difficult.
Stage 3: Thawing
Shoulder motion slowly improves during the “thawing” stage. Complete return to normal or close to normal strength and motion typically takes from 6 months to 2 years.
In frozen shoulder, the smooth tissues of the shoulder capsule become thick, stiff, and inflamed.
CAUSE
The causes of frozen shoulder are not fully understood. There is no clear connection to arm dominance or occupation. A few factors may put you more at risk for developing frozen shoulder.
Diabetes. Frozen shoulder occurs much more often in people with diabetes. The reason for this is not known. In addition, diabetic patients with frozen shoulder tend to have a greater degree of stiffness that continues for a longer time before “thawing.”
Other diseases. Some additional medical problems associated with frozen shoulder include hypothyroidism, hyperthyroidism, Parkinson’s disease, and cardiac disease.
Immobilization. Frozen shoulder can develop after a shoulder has been immobilized for a period of time due to surgery, a fracture, or other injury. Having patients move their shoulders soon after injury or surgery is one measure prescribed to prevent frozen shoulder.
PREVENTION
One of the most common causes of frozen shoulder is the immobility that may result during recovery from a shoulder injury, broken arm or a stroke. If you’ve had an injury that makes it difficult to move your shoulder, talk to your doctor about exercises you can do to maintain the range of motion in your shoulder joint.
EXERCISE
TREATMENT
Frozen shoulder generally gets better over time, although it may take up to 3 years. The focus of treatment is to control pain and restore motion and strength through physical therapy.
Your doctor might recommend other kinds of treatments, including:
- A corticosteroid injection in your shoulder joint reduces your pain and improve your range of motion.
- Non-steroidal anti-inflammatory medicines. Drugs like aspirin and ibuprofen reduce pain and swelling.
- Steroid injections. Cortisone is a powerful anti-inflammatory medicine that is injected directly into your shoulder joint.
Good management of pain, and careful control of compensatory movements can help you to minimise the negative effects of the condition.
Long term abnormal movement patterns of the shoulder can cause postural asymmetries, neck and back pains. So be vigilant with monitoring your posture. Make sure you stand up straight when moving your arm, and do not overcompensate by leaning your body as you lift your arm.
Try to minimise just how much you hunch your shoulder up.


